These days, when Chicago's doctors confront ill health, they deploy a medical arsenal ripped from the pages of a sci-fi novel. Some MDs, the so-called Nintendo docs, use robotics for prostate, heart bypass, and other surgeries-or they dispatch mechanical messengers on a fantastic voyage through a patient's veins. Other doctors focus their energies on the research lab, exploring the worlds of genetics and synthetics, drug trials and bioengineering to discover new ways to combat trauma, cancer, and lost limbs. The following pages detail these cutting-edge advances and treatments-advances that put Chicago in the front ranks of medical innovation.
| 01 |
Limb Replacement
Rehabilitation Institute of Chicago, Todd Kuiken
 |
|
Mitchell commands her new bionic arm simply by thinking about what she wants it to do-just as she had done with the arm that she lost. |
Journalists can be a cynical bunch, but even they were awed this past September when doctors at the Rehabilitation Institute of Chicago (RIC) introduced them to a former marine named Claudia Mitchell, who had lost her left arm in a motorcycle accident. Now, here she stood with her new bionic arm, demonstrating that she could reach over her head, flex her hand, or turn her wrist simply by thinking that she wanted to perform those acts-just as she had done with the arm that she lost.
The biomedical engineer behind this futuristic happy ending is Todd Kuiken, the director of the neural engineering center for artificial limbs at RIC, who has spent the past 20 years striving to improve motorized artificial arms. In Mitchell's case, Kuiken and Gregory Dumanian, a plastic surgeon at North-western Memorial Hospital, took the five major nerves that controlled the former marine's hand and arm and grafted them onto her pectoral muscles. From there, the nerves send signals to her new arm and hand, directing it to do whatever Mitchell is thinking (within the still-limited capacity of the mechanized prosthetic).
Now the U.S. Department of Defense plans to begin offering these robotic arms to wounded soldiers. As for Kuiken-whom Chicago selected as one of its Chicagoans of the Year for 2006 (see City Lights)-his next objective is creating a bionic leg.
| 02 |
Endovascular Surgery
Rush University Medical Center, Demetrius Lopes
 |
|
Demetrius Lopes |
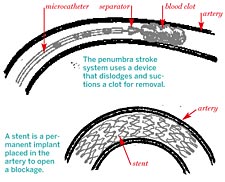
Demetrius Lopes, a neurosurgeon at Rush University Medical Center, is a prime example of the "Nintendo generation" of doctors. To remove a blood clot or repair a burst blood vessel in the brain of a stroke patient, Lopes begins by making an incision in the patient's thigh. Then, using a joystick or touchpad to direct movement, he sends a catheter carrying a tiny device through the patient's circulatory system, tracking its course via a three-dimensional image projected on a video screen. Once the device has arrived at the point in the brain where the stroke occurred, Lopes can use it to suction out a blood clot; break up a clot and carry it out; or insert a small, flexible stent to repair or strengthen a blood vessel.
"[Blood vessels] are natural expressways inside your body," Lopes says. "We can do all the surgery now from inside your veins. It's not necessary anymore to cut open your skull after a ‘brain attack.'" And this minimally invasive procedure reduces recovery time from eight weeks to 12 days.
|
Illustrations by John Kenzie
 |
Though doctors have been using endovascular (defined as "within the blood vessels") surgery for some time to treat other parts of the body, Lopes is among those pioneering its use in the brain. As a consultant to Siemens, the medical equipment manufacturer, he also helps develop the equipment that makes these innovative procedures possible. "It's not a revolution you can deny," says Lopes, the Brazilian-born son of a neurosurgeon. "It's a revolution that's here. I'm 36, and more has changed in this field since I started than in my father's entire career."
| 03 |
Preventing Strokes
University of Illinois Medical Center, Fady Charbel
|
Photograph: Courtesy of University |
|
UIC's Fady Charbel with the NOVA technology |
In the past, when diagnosed with the potential for a stroke, patients often underwent preventive surgery. Now a two-year study conducted by the University of Illinois Medical Center at Chicago has demonstrated that two-thirds of those high-risk patients could actually forgo surgery and manage their condition with drug therapy.
The study was an offshoot of work conducted by Fady Charbel, head of neurosurgery at UIC, who last April patented software-called Noninvasive Optimal Vessel Analysis-that helps doctors measure blood flow in individual blood vessels of the brain. Whereas MRI technology could determine only the presence or absence of blood flow, NOVA measures its volume and direction, while also providing a multidimensional view.
| 04 |
Saving the Brain
Northwestern Memorial Hospital, Ali Shaibani and Tim Carroll
|
Photograph: Courtesy of Northwestern Memorial Hospital
 |
|
Ali Shaibani |
 |
|
Shaibani and Carroll's innovation helps doctors gauge blood flow to a damaged brain. |
When confronted with a stroke victim, doctors essentially have had to guess where brain tissue had been irreparably damaged and where it might be saved. Now, combining their complementary backgrounds, Ali Shaibani and Tim Carroll of Northwestern Memorial Hospital have come up with a way to eliminate the guesswork.
Shaibani, an MD trained in interventional neuroradiology and neurosurgery, gives much of the credit to Carroll, a professor trained in high-energy physics and medical imaging. Other researchers, he says, had unsuccessfully attempted to develop ways of quantifying blood flow to a damaged brain, which would help doctors determine which parts of the brain could be salvaged. But it was Carroll who finally devised a mathematical model that, coupled with MRI technology, actually created an effective technique-which Shaibani calls quantitative MR perfusion.
"We need to know what parts of the brain are irreparably damaged and will get no benefit from treatment," says Shaibani. That way, he says, precious time isn't wasted on futile attempts at therapy. Instead, doctors can now effectively determine which parts of the brain can still be salvaged using a clot-dissolving agent.
| 05 |
Aneurysms
Northwestern Memorial Hospital, Ali Shaibani and Tim Carroll
Next up for the Carroll-Shaibani team: finding a way to measure the likelihood that a brain aneurysm will burst. Doctors often spot a developing aneurysm when performing a scan for sinus diseases and other problems of the head. But it's still something of a guessing game to determine when the aneurysm might burst. While other researchers are looking at size and location, Shaibani and Carroll are using fluid dynamics-which measures how an aneurysm expands as blood pulses through it-to calculate the thickness of the aneurysm wall. They estimate that the process, called pulsatility imaging, is about five years from fruition.
| 06 |
Diabetes
University of Illinois Medical Center at Chicago, Jose Oberholzer
|
Photograph: Courtesy of University of Illinois
Medical Center  |
|
Islet cells containing insulin |
Since 2004, hopes for a functional cure for diabetes have centered on the Chicago Project. Led by Jose Oberholzer, the director of cell and pancreas transplantation at the University of Illinois Medical Center at Chicago, the international effort includes doctors and scientists from France, Switzerland, Italy, Israel, Canada, and the United States. Doctors, however, are dependent on a limited number of pancreases from deceased donors-which is why Oberholzer is trying to multiply the number of crucial islet cells once they are harvested from a pancreas.
"This is not an easy endeavor," Oberholzer says. "When you make them grow, you may induce changes that make the cell less functional. You may even create a cancer cell. It's been tedious work for ten years now."
 |
|
Jose Oberholzer |
Should he succeed, Oberholzer would solve one significant problem related to islet transplantation. Today, 20.8 million diabetics need islet cells, but each of the 6,000 annual donors can help only one diabetic. Oberholzer is currently trying to double and triple the number of diabetics that can be helped, but he hopes to one day make the cells multiply by the hundreds. The next stage of the project entails protecting the implanted islet cells so that the body doesn't reject them as alien invaders. After successful trials with animals, Oberholzer and his Chicago Project collaborators have begun human testing in Italy with promising results.



