In 1904 in Australia, a man known as Mr. Doodeward acquired a stillborn two-headed child and displayed it in a traveling freak show. To his surprise, police confiscated the specimen, claiming the exhibit was obscene. When Doodeward claimed the two-headed baby was his property, and sued to get it back, the judge faced a perplexing question that haunts courts even today: Can anyone own a human body or its parts?
The judge knew that if he ruled the corpse was not Doodeward’s property, then police might have to confiscate bodies from museums, medical institutions, and archaeologists. Unwilling to open that Pandora’s box, he ruled that if a corpse or part of a corpse had been altered for science or medicine, it acquired value and became property. Doodeward’s specimen, the judge ruled, had been altered by being preserved in formaldehyde. Mr. Doodeward got back his two-headed baby.
The logic in the ruling—that only those who scientifically transform bodies or body parts can own them—reverberates through courtrooms and medical facilities today, often in ways that boggle the mind. In the 1980s, for instance, doctors at the University of California, Los Angeles, who were treating a leukemia patient discovered that certain chemicals in his blood had special curative powers—so special, the university patented them and made millions selling the rights to a biotech company, all without the knowledge of the patient, John Moore. When Moore sued, and his lawyer made the seemingly reasonable argument “that a patient owns his body, his own tissue, his own DNA,” the California Supreme Court disagreed. What happened to Moore might have been unethical, the justices ruled, but it was not illegal: People, the court said, have no property rights to their own bodies.
****
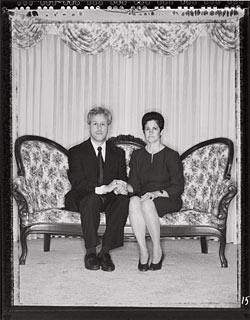
That view persists even now, despite the fact that human body parts, such as Moore’s cells, can be worth a fortune to the multibillion-dollar biotechnology industry. In part because the stakes are so high, patients are fighting ever harder for the rights to their own body parts. Some of the legal wrangling has centered on human genes—including a court battle waged by Dan and Debbie Greenberg of south suburban Homewood. The Greenbergs had two babies with Canavan disease, an inherited brain disorder that usually kills in childhood. In the 1980s, the Greenbergs persuaded a doctor to try to find the gene that caused Canavan. Along with dozens of other families, they gave him money and samples of blood, urine, and tissue—even autopsy samples after their first child died. To everyone’s amazement, the doctor identified the Canavan gene in 1993.
A triumphant ending—until the families discovered that the doctor and his employer, Miami Children’s Hospital in Florida, had patented the gene. The implications left the families shocked: The hospital had dominion over who could use the gene and how—from researchers who wanted to use it to find a cure for Canavan, to lab directors who wanted to administer carrier or prenatal tests. It could profit off the gene, too: By one estimate, the hospital is earning about $375,000 a year from charging royalties on every test involving the Canavan gene. (A hospital spokesperson disputed this figure, saying the revenue is significantly less.)
The commercialization of the gene infuriated the Greenbergs and the other families who had made such painful, personal contributions to its discovery. After unsuccessfully negotiating with the hospital, they filed a lawsuit. “I gave myself and my son and anything [the doctor] wanted to help wipe out this disease,” says Frieda Eisen of Brooklyn, New York, whose son, Jacob, had Canavan. “I thought it was more of a donation for the common good of mankind, not for a hospital to profit on. Jacob was as much a part of this discovery—all the children were—as the hospital. Why should they make money on my child, on everything my child donated?”
That’s a question the courts may decide. Greenberg, et al. v. Miami Children’s Hospital, et al., filed on October 30, 2000, in federal district court in Chicago, is commanding attention because it may help establish new rules for the ownership of human genes. The suit contends that without the families’ informed consent, the hospital had no right to patent a gene that was discovered using the patients’ body samples. In a particularly fortunate turn for the plaintiffs, the case has been transferred to Florida, a state that has swept aside the archaic legacy of Doodeward and stepped into the brave new biotech world. Under Florida law, people do own their own body parts, and a particular statute protects their DNA. “That statute could make things interesting,” says one of the plaintiffs’ pro bono lawyers, Lori Andrews.
****
The Greenbergs first held their newborn son, Jonathan, in Ingalls Memorial Hospital on June 12, 1981. “He was beautiful,” Debbie says. “He looked perfect.” An occupational therapist who works with children, Debbie had dreamed of this day since her lonely upbringing in Peoria. “Ever since I can remember, I wanted to be the mother of a large family,” she says. “I wanted two boys and two girls.”
Dan, a real estate lawyer, had gone queasy during his wife’s labor. But his world righted as he took his first glimpses of Jonathan’s dark eyes and thatch of black hair, features that reflected the Greenbergs’ proud eastern European Jewish ancestry. What’s more, the baby had excellent timing, arriving on the couple’s fourth wedding anniversary. “We couldn’t have asked for a better gift,” says Dan, who was 26.
Dan had met Debbie during her freshman year at the University of Illinois at Urbana-Champaign. A handsome, curly-haired sophomore, he liked Debbie’s fun-loving nature and shared her desire to start a family. The two married in 1977, though Debbie had about a year left of college. “We were really in love,” she explains. “And I had my goals in life set: I’m getting married and having lots of kids.”
That fall, Dan attended law school at DePaul University in Chicago, while Debbie finished the clinical portion of her occupational therapy program at the University of Illinois at Chicago. In the evenings, they dreamed of a house with many bedrooms—and cooing babies to fill them.
By 1979, Dan had passed the bar and taken a job with a Chicago Heights law firm. The Greenbergs’ dreams began to come true: They bought a four-bedroom house in Park Forest, and in September 1980, Debbie learned she was pregnant, after just four months of trying. “I was elated,” she says. “I was sick as a dog, but it didn’t matter.”
At the time, Debbie worked with physically and mentally disabled children, alongside several other therapists in various stages of pregnancy. She found herself calculating the frightening odds she had learned in one of her college courses: “I remember thinking, At least one of us is going to have a child with some sort of disability.”
She took comfort in knowing that her baby wouldn’t inherit Tay-Sachs disease, a dreaded neurological disorder common to Jews of eastern European origin, known as Ashkenazi Jews. A blood test in college had determined that Debbie didn’t carry the mutant recessive gene that causes it.
Still, when Jonathan arrived in 1981, she grew worried when he couldn’t latch on to her nipple. “The nurse just said, ‘Oh, some babies are tired after the hard work of labor,’” Debbie recalls. But later, when no one was in the room, she clapped loudly near Jonathan’s head to measure his startle reflex. “Most newborns just jerk; it’s a normal response,” Debbie says. “But he would just start screaming. That’s not normal at all.”
The crying persisted at home. Only holding Jonathan kept him quiet, so Dan or Debbie carried him nearly 24 hours a day. By the time he reached two months, he still couldn’t hold up his head, follow motion with his eyes, or reach for toys. “You’re a first-time, neurotic mother,” a doctor told a concerned Debbie during Jonathan’s two-month checkup. “You have a beautiful baby; take him home and enjoy him.”
By six months, Jonathan was still functioning at a newborn’s level: He could not sit, roll over, make eye contact, grasp objects, or control his enlarged head. Even worse, the muscles in his hands had involuntarily contracted into clenched fists, as if he were locked in a rage from which he couldn’t break free. Distraught, Debbie found a new doctor. This one barely had to glance at Jonathan before packing him off to Children’s Memorial Hospital in Chicago.
There, Cynthia Stack, a pediatric neurologist, greeted Debbie and Dan in a clipped, professional tone. But when she examined Jonathan, Stack softened. “I think I know what you have,” she whispered in the baby’s ear, “but I sure hope I’m wrong.”
She wasn’t. After weeks of tests, the Greenbergs returned to Stack’s office to hear the diagnosis. By process of elimination, the doctor had determined that Jonathan had Canavan disease—a rare genetic disorder that, like Tay-Sachs, is more common among Ashkenazi Jews (who make up 90 percent of the U.S. Jewish population). Like the rest of the medical community, Stack knew frighteningly little about the disease: Passed on by a defective gene, the disorder causes the brain’s nerve-protecting white matter, called myelin, to turn spongy, leading to the deterioration of the baby’s central nervous system. “There isn’t a cure,” Stack told the Greenbergs. “He probably has a two- to three-year life expectancy.”
Dan and Debbie listened in shock. “I was in a state of total disbelief,” Debbie recalls. “I had still been hoping it was ‘just’ cerebral palsy.”
Joel Charrow, a geneticist at Children’s Memorial, delivered the second blow. The Greenbergs, he explained, had passed Canavan on to Jonathan via a mutated gene that both of them carried. Many Ashkenazi Jews—about one in 40—carry the gene. The carriers, including Debbie and Dan, are healthy; the disease occurs only when a child inherits the mutated gene from each parent. So, Charrow continued, every baby the Greenbergs conceived would have a one in four chance of inheriting Canavan. And because no prenatal test existed, the Greenbergs would have no way of knowing if a baby was afflicted until it was born and the disease’s devastating symptoms began to appear.
Driving south on Lake Shore Drive toward home, Debbie sobbed in the passenger seat. She cried for her son, who would die of a terrible, ill-comprehended disease. And she cried for herself and the family she might never have. With only a 75-percent chance of bearing healthy children, becoming the mother of a large family meant taking her chances in a dangerous game of Russian roulette.
Twenty years later, Charrow remembers the meeting with the Greenbergs. “I think Canavan disease, like Tay-Sachs, has got to be one of the worst experiences a family can go through,” he says. “When the baby is born, he looks normal. So the parents for a few months have what appears to be a normal child, after which the baby stops learning, and may not feed very well, and things go downhill from there. To have to witness your child’s deterioration over a period of years has got to be excruciatingly painful.”
At home, hopelessness set in. “I asked myself all the time, How could God do this to me?” says Debbie, who all but renounced her religious faith. Dan assuaged his grief by digging up what little information existed on Canavan. Ultimately his research led him to the National Tay-Sachs & Allied Diseases Association, a nonprofit organization founded in 1956 for families of children with Tay-Sachs and some 40 other genetic diseases, including Canavan.
While nothing could help Jonathan, the Greenbergs funneled their energies into helping prevent Tay-Sachs. With several other families, they founded the Chicago chapter of the Tay-Sachs association and organized low-cost blood screenings for the Tay-Sachs gene, in Jewish community centers and medical school clinics. “The word wasn’t out on the street,” Dan says. “Jewish people weren’t getting tested to see if they were at risk for having a child with Tay-Sachs.”
At screenings, a vial of blood was taken from each participant and, for a minimal cost, processed later in a lab. If a person was identified as a carrier, he or she would know that by conceiving with another carrier, the baby would have a 25-percent chance of having Tay-Sachs. Since the carrier screening program was started in the seventies, it has tested more than one million people, and the incidence of the disease has dropped by 90 percent among Ashkenazi Jews.
In Chicago, fundraisers and donations helped keep the test at its bargain-basement price. So did the generosity of Reuben Matalon, a geneticist and a professor at the University of Illinois at Chicago, who told Dan he would do the blood testing at his UIC lab, where he would charge $10 a test, far cheaper than the usual $50 fee.
Meanwhile, Debbie and Dan decided to bet on the 75-percent chance that their next baby would be fine. But Amy Greenberg, born in 1983, had Canavan disease, too.
Now Debbie and Dan had two terminally ill children who would never develop beyond the infant stage. Despite their disabilities, the children could smile, laugh, and recognize Dan’s and Debbie’s voices. When their parents made high-pitched noises, blew on their faces, or administered noisy raspberries to their bare legs, the children burst into giggles. “We lived for those smiles,” Dan says. “Those are what got us through.” Ultimately, however, caring for children who could not move or feed themselves proved too draining. The Greenbergs placed Amy and Jonathan in the South Side branch of Misericordia, a full-time residential care facility administered by nuns.
Visiting twice a week, Dan hoped that a researcher might grow interested in Canavan disease, which had never managed to command serious attention from scientists. And as he got to know Reuben Matalon, Dan sensed he had found his scientist. “My feeling was that he had such a big ego and was always feeling that he should be at the top,” Dan recalls. “So I thought, If he hears someone else is doing some really good research, maybe he’ll say, ‘Hey, wait a minute; I’m not going to be outdone.’ And that’s pretty much what happened.” (Matalon told Chicago his lawyer advised him not to comment for this story.)
In May 1987, Dan talked to Matalon about a researcher working to unravel the Canavan mystery, and Matalon began to pepper him with questions. Soon the doctor wanted blood and urine samples from Jonathan and Amy. “He became sort of obsessive-compulsive about getting samples,” Dan says. “First, we had Misericordia take the samples and send them to him. Then, he wanted more samples—so badly that he went to go get them himself.”
Research can often take years of fruitless labor, but with-in months Matalon told Dan, “I think I’m finding something here.” But the doctor needed more blood, urine, skin, and even autopsy samples to further his research, so Dan put him in touch with other parents of children with Canavan. “And not long after,” Dan says now, sitting at his kitchen table in Homewood, “Matalon found the needle in the haystack that nobody could find.”
The needle was an enzyme called aspartoacylase, which was missing in the brains of all the Canavan children. To announce his breakthrough, Matalon summoned the Greenbergs and two other Canavan families to his office at UIC. With an in-depth slide presentation, he showed how the deficiency of aspartoacylase led to a buildup of another chemical, n-acetyl aspartic acid. This chemical imbalance caused damage to the brain’s white matter, ultimately triggering the devastating condition of Canavan disease.
With this discovery, Matalon thought, reliable prenatal tests could be performed by testing the enzyme levels of the fetus. “We were so excited,” says Debbie. “Now we didn’t have to feel envy that the Tay-Sachs parents had prenatal testing and we didn’t.”
Matalon walked the elated families to his lab, explaining that he wanted to start work on developing a carrier test. To that end, he asked permission to take skin samples from each of the parents. They agreed, and after completing the biopsies, Matalon took the six parents to lunch—where they celebrated the doctor by ordering “Reuben” sandwiches.
Debbie got pregnant within months, though she and Dan decided that if a prenatal test showed the fetus had Canavan, they would abort the pregnancy. But when a test performed at ten weeks showed normal enzyme levels in the fetus, Debbie says, “we were overjoyed beyond belief.” (Several years earlier, the Greenbergs had adopted two baby girls, Stephanie and Michelle.)
On February 13, 1989, Debbie gave birth to an eight-pound boy, Joshua. “For the first few weeks, I watched him constantly for signs of Canavan,” she says. “I just didn’t believe the prenatal testing.” But he had no trouble nursing from Debbie’s breast, and by three weeks he was smiling—far sooner than Jonathan and Amy. At three and a half months, Josh rolled himself over twice in one day, and Debbie felt as if she had witnessed a miracle. “Jonathan and Amy had never rolled over, not once,” she says. “I breathed a huge sigh of relief. For the first time, I knew I had given birth to a healthy baby.”
In 1989, Matalon took a prestigious new job: director of research at Miami Children’s Hospital—whose financial support and new, state-of-the-art facilities would increase his chances of identifying the Canavan gene. There Matalon continued administering the prenatal test, charging expectant couples between $100 and $200, according to Rajinder Kaul, a geneticist who worked closely with Matalon in Miami. After ten negative prenatal tests and ten healthy births, including Joshua’s, lightning struck: Four families in the early nineties bore children afflicted with Canavan—despite negative tests. The tragedies resulted in two lawsuits against Miami Children’s Hospital, which settled both out of court.
With the tests discontinued, Matalon urgently searched for the gene that caused Canavan—if it were known, technicians would need only basic equipment to examine the DNA of a prospective parent or a fetus to determine whether the Canavan gene had the disease-causing mutations.
Like a small town banding together to search for a lost child, everyone pitched in. The Greenbergs and other families provided more blood samples. Both the Canavan Foundation and the United Leukodystrophy Foundation sponsored a program to obtain further blood samples. Rabbi Josef Ekstein, the head of Dor Yeshorim, an organization devoted to the prevention of Jewish genetic diseases, persuaded several reluctant families with Canavan children to give samples. And Frieda Eisen trekked from Brooklyn to Miami every year with her son Jacob, for MRIs and “any other testing Matalon wanted.”
“I was very gung ho,” says Eisen. “Everything revolves around these children: their feeding and diapering and therapies. I wouldn’t want anyone to go through the pain and suffering and heartache I went through.”
The Greenbergs had already made a particularly painful donation to Matalon in 1992, when 11-year-old Jonathan died. Though grieving, they immediately ordered an autopsy and gave Matalon pieces of their son’s brain and other vital organs.
Finally, in 1993, Matalon and his researchers isolated the Canavan gene. “He called me to tell me the news, and it was worth more than a million dollars to me,” recalls Rabbi Ekstein. “I thought he deserved a medal.” For a news conference extolling the breakthrough, the hospital flew in at least one of the families who had contributed to the research. Just before the event, one moment captured the indispensable role of the families. Guang Ping Gao, one of Matalon’s researchers, met Frieda and Jacob Eisen in a hallway. “I cloned his gene,” Guang said softly, touching the frail boy, who sat in a thickly padded stroller. “I held his gene in my hand. It’s nice to meet him.”
Later, Matalon announced his findings, including the DNA sequence of the gene, in the journal Nature Genetics. With the sequence now public knowledge, reliable DNA-based prenatal tests could be performed at almost any lab. Not long after, Matalon used some 5,000 blood samples from Dor Yeshorim, among other donors, to do further research and develop a reliable carrier test.
Doctors, hospitals, and community organizations around the world began offering the tests, sending blood samples to labs for screening. In 1996, the Canavan Foundation offered free testing at Mount Sinai Hospital in New York. Rabbi Ekstein’s organization alone tested more than 13,000 people a year. In 1998, the American College of Obstetricians and Gynecologists made offering the test to pregnant Ashkenazi couples, or those contemplating pregnancy, a “standard of care” that rendered obstetricians who did not offer the test liable if their patient bore a child with Canavan. “That really resulted in a dramatic increase in the number of couples being tested,” says Judith Tsipis, director of the genetic counseling program at Brandeis University, who worked on getting the standard of care protocol.
Tsipis isn’t sure that what happened next was entirely coincidental. A few weeks after the “standard of care” announcement, Rabbi Ekstein received a letter from lawyers for Baylor University, whose laboratory processed some 5,000 Canavan tests a year for him. “It said that the samples sent last week would not be tested,” Ekstein recalls, “and that no future samples would be tested.” He learned why in a subsequent letter from Miami Children’s Hospital: In October 1997, it read, Matalon and the hospital had been granted a patent for the gene that, when mutated, was responsible for Canavan disease—a patent the hospital’s lawyers intended to vigorously enforce.
From that day Miami Children’s Hospital would not allow any further testing by labs without a license from the hospital. The free testing days at Mount Sinai, for instance, would have to be discontinued. What’s more, the patent empowered the hospital to charge a royalty—at the time, $25; now $12.50—for every prenatal or carrier test performed. And the hospital limited the number of tests that could be done. That was a far cry from the Tay-Sachs gene and tests; although they were also patented, the holder had donated the patent to the public good. Thus, any lab could test for the Tay-Sachs gene, and no royalty fees were collected—which, say researchers, is one reason why today only five Tay-Sachs babies are born a year, down from 50 in the 1970s.
“I called Matalon and said, ‘Can you get us out of this problem?’” Rabbi Ekstein says. “Matalon said he had signed an agreement with the hospital and that he was handcuffed. I told him, ‘You’re a fool.’ And he agreed with me.”
Rajinder Kaul, now a geneticist at the University of Washington, recalls a different set of circumstances. He claims it was Matalon’s idea to patent the gene in the first place. “I was there when he said it,” Kaul says. “This hospital was new; it didn’t know anything about patenting genes.”
Matalon has said he has not profited from the patent. “My contract said every invention I make would be theirs,” he told The New York Times. “I am not in the inventing business. I am a research person. If they make money on me, I don’t care.”
Still, Matalon’s public statements regarding the contributions of Dan Greenberg changed dramatically over the years. In 1993, Matalon was quoted in a press release as saying, “This is a disease where a partnership between researchers and the families of affected children is critical for advancing knowledge. . . .” But when Jon Merz, a professor of bioethics at the University of Pennsylvania, interviewed Matalon seven years later for an article, the doctor said that Greenberg had played “no role” in the discovery of the gene.
Regardless of whether Matalon or Mi-ami Children’s was the driving force behind the patent, the doctor and the institution eventually parted ways. The hospital shut down its genetics labs; Matalon left in June 1996 and now runs a lab at the University of Texas in Galveston. “I feel like he is the cow who gave the milk and then spilt the bucket,” says Rabbi Ekstein. “He did this wonderful thing, and then he made a big mess.”
To Professor Merz, the hospital and Matalon have ignored the contributions made by the Greenbergs and other families who donated blood and tissue. “The only irreplaceable, ‘critical’ resource . . . in the discovery of the gene was the participation of the affected families,” Merz writes in his book Who Owns Life? “The system, in the end, fails to acknowledge their status and their contribution. It is, in a very real way, ‘their’ gene; yet not.”
A few labs signed Miami Children’s licensing agreement in order to make the Canavan tests available. But several labs, like the one at the Hospital of the University of Pennsylvania, went out of the Canavan testing business altogether rather than sign what one lab director has called “a wretched contract.” Baylor’s lab stopped all Canavan testing for several months—a particular burden for Dor Yeshorim, whose Rabbi Ekstein found it impossible to get another lab to process his samples for the same low price he had wangled from Baylor. Ekstein says he has had to cut back significantly on Canavan testing.
Today, Miami Children’s Hospital has granted 15 labs a license to offer the Canavan test, which costs about $200 in Chicago and upwards of $400 in other cities. The hospital also has patented the gene in Israel.
As for its $12.50 royalty fee, Miami Children’s says it uses the money it earns on each Canavan test for further pediatric research. “We do not expect to ever recoup the millions and millions of dollars we spent that resulted in this medical breakthrough,” the hospital said in a written statement to Chicago.
What’s galling to Dan Greenberg and the other plaintiffs in the lawsuit is that there are any restrictions or royalties at all. “To me, a gene is like a raw material,” Greenberg says. “You can’t patent iron ore. You find it in the ground; it’s there; it’s a natural product on earth. Well, the genes in my body are also a natural product. And for somebody to be able to prevent anyone from using this raw material, even from doing tests on it—that’s what I just think is terrible and wrong.”
Unfortunately for the Greenbergs, there has been legal precedent for patenting a gene since a landmark 1980 Supreme Court ruling, which established that living organisms altered or isolated by “the hand of man” could be patented, provided that the inventor did something new and useful with the discovery. Since then, about 500,000 gene patents have been granted or are pending, according to the advocacy group GeneWatch UK.
In discovering the Canavan gene, Dr. Matalon identified its DNA sequence and then isolated the gene from its chromosome. Because that DNA sequence doesn’t naturally occur in an isolated form, and is thus considered new, it is eligible for a patent. In addition, Matalon found specific uses for the isolated gene—prenatal and carrier tests and gene therapy, among others—so the gene is considered useful.
Given that, the plaintiffs, as much as they despise the patent, aren’t challenging the legality of it—“only the fraudulent way in which it was obtained,” says their lawyer, Lori Andrews, a professor at the Chicago-Kent College of Law.
Their case rests on several grounds, the strongest of which is an alleged lack of informed consent. For the first few years of the research, Matalon took blood and other samples without written consent forms from the Greenbergs and other families. The suit claims this breached his duty as a medical researcher to provide the participants with information that might have influenced their decision to participate in the research.
Not until February 1994 did the hospital send out a consent form, signed by Matalon, for the families to sign. But it misrepresented Matalon’s purpose, Andrews argues. The form did not say that Matalon intended to use the genetic information to patent the Canavan gene for commercial use. It stated simply that Matalon’s research purpose was: “To identify mutations in the Canavan gene which may lead to carrier detection.” The plaintiffs, Andrews contends, would never have cooperated with Matalon had they known their genetic information would be used to patent the gene for a commercial purpose.
Miami Children’s Hospital would not comment on the patent or the lawsuit directly, but it did acknowledge the families’ contributions. “It’s important to note that when the research began, there were no stipulations attached to their donations,” the hospital said. “It is our understanding that many families worked closely with Dr. Matalon on the research and that they, along with other families, voluntarily provided Dr. Matalon and other doctors with the research samples. This was all done in the spirit of cooperation.”
Under law in Florida, where the case will be tried, the results of any DNA analysis of an individual “are the exclusive property of the person tested.” Andrews thus will argue that the defendants committed property conversion—using property given for one purpose for a different purpose. “The Greenbergs gave permission for one use of their tissue and genetic information—their property—which was to discover the Canavan gene,” says Andrews. “But they never agreed to other uses, such as gene patenting and commercialization.” Andrews draws the analogy that giving your car to your mechanic to investigate a problem doesn’t mean the mechanic has a right to sell the car, or its parts, and keep the money.
The suit asks for damages—money that, Dan Greenberg says, “will be put in a trust and used for education and for public screenings, so people can get tested for a reasonable cost.” But ultimately, what is driving this suit is not so much money as feelings of betrayal. Although Dan had worked closely with Matalon for years—“There were days I talked to him more than I talked to my wife,” he says—Matalon had never mentioned patenting the gene. “The whole time, he would always talk about how he was doing this to spare people these tragedies in their lives,” says Dan. “So for him to turn around and commercialize the gene, that to me is a desecration of all the good that came out of Jonathan and Amy’s lives.”
Showing videos of Amy to a recent visitor, Debbie and Dan smiled wistfully. Unusually pretty, their daughter had flawless skin and thick brown hair, glistening with highlights. She died in 1999 in her parents’ arms, just a few months after her 16th birthday. There is still no cure for Canavan. “You know,” says Dan, “at one time people were scientists for the sake of discovering things and having the honor of helping people via those discoveries. I respect that the dollar does drive certain people to accomplish things, but where is that purist research that people used to do, simply to help?”
That kinder, gentler era of medicine may have gone the way of the sugar-cube vaccine. Recently, a group of patients with PXE—a genetic disorder that attacks the connective tissue—pushed for research that eventually uncovered the disease-causing gene mutation. Like the Greenbergs, the PXE patients recruited other families to supply blood samples. But the families, through a foundation, set up their own blood bank, controlling researchers’ access to it. They also retained rights as coinventors on the gene patent and negotiated a license that ensured testing would be widespread and affordable. Lori Andrews puts it this way: “These people are saying, ‘What happened to the Canavan people, we don’t want to happen to us.’”


