Last week, Princeton economist Anne Case, along with her colleague and husband Angus Deaton, himself the most recent Nobel laureate in economics, discovered something astonishing (emphasis mine): "a marked increase in the all-cause mortality of middle-aged white non-Hispanic men and women in the United States between 1999 and 2013. This change reversed decades of progress in mortality and was unique to the United States; no other rich country saw a similar turnaround."
The finding is getting a lot of attention. But it shouldn't be a complete surprise. I was instantly reminded of the crushing piece "What's Killing Poor White Women?" by Monica Potts, and the research that inspired it, led by Jay Olshansky, a professor of epidemiology at UIC's School of Public Health.
As the title of Potts's article suggests, Olshansky and his co-authors had hit on a dramatic finding: "For those with less than a high school education, white males and white females experienced a consistent pattern of decreasing longevity, while blacks and Hispanics of both sexes exhibited increasing longevity."
Life expectancy at birth for white, female high-school dropouts in 1990 was almost 79 years of age. By 2008, it had fallen to just over 73 years. For white, female high-school graduates, life expectancy grew very slightly; for college graduates, it grew significantly. As Potts wrote at the time, "the last time researchers found a change of this magnitude, Russian men had lost seven years after the fall of the Soviet Union, when they began drinking more and taking on other risky behaviors." Yet there was no such cataclysmic event to explain this change.
"At the time, we were speculating that it might be nonprescription drugs and alcohol consumption. We didn't know at the time," Olshansky told me this week. "[Case and Deaton] confirmed what it was—which was, in fact, higher mortality associated with nonprescription drug use."
Mortality Rate Changes
First, here are the changes in mortality rates for Americans ages 45-64, according to Case and Deaton's study. Notice how the white non-Hispanic group is the only one that increases.
.png)
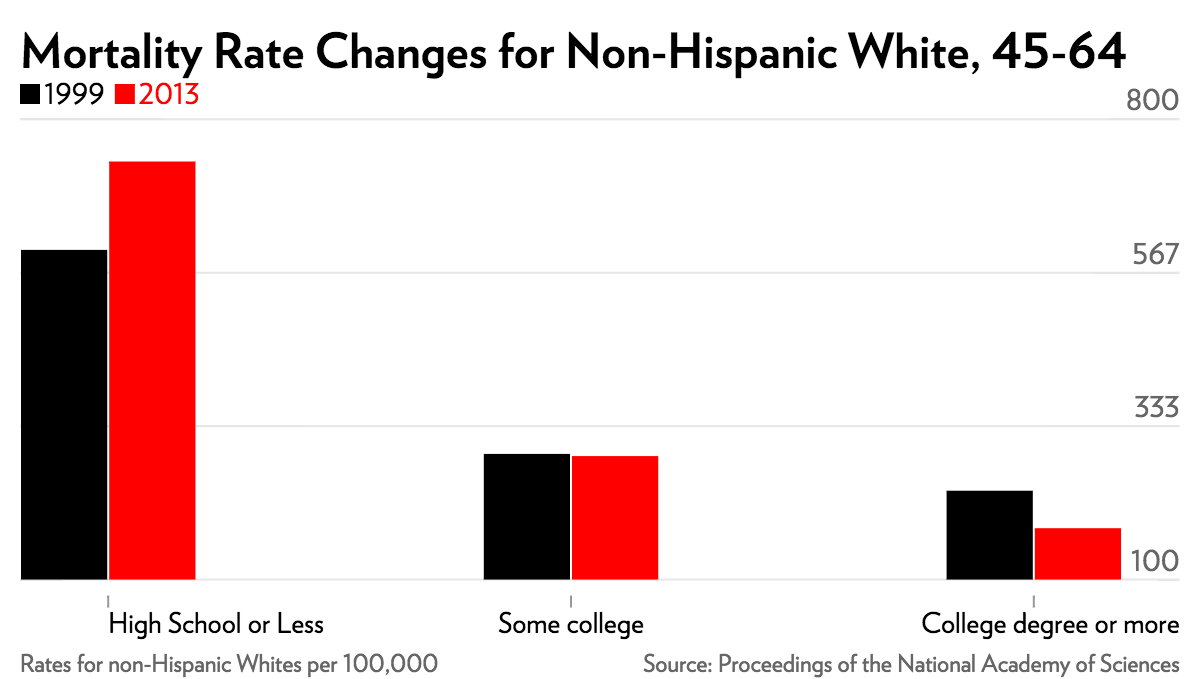
But that's not the whole story. Take a look at just the white non-Hispanic group by education level.
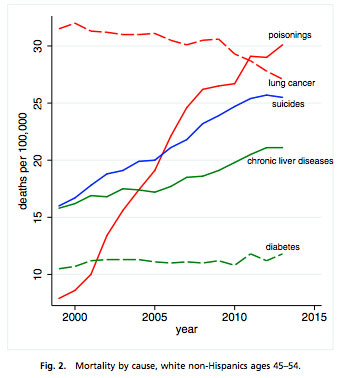
And even that's not the full story of what's happening. For that, the authors looked at what causes of death were increasingly dramatically over that period. For whites of both sexes, ages 45 to 54 with a high-school education or less, the authors write, "the mortality rate from [drug and alcohol] poisonings rose more than fourfold for this group, from 13.7 to 58.0 [per 100,000], and mortality from chronic liver diseases and cirrhosis rose by 50 percent."
For the same group, mortality by intentional self-harm rose from 21.8 to 38.8 per 100,000. Chronic liver cirrhosis rose from 26.7 per 100,000 to 38.8 per 100,000. Yet poisonings from drugs and alcohol—overdoses, essentially—rose staggeringly. Take a look at the chart on the right.
Yet Olshansky has been expecting something very much like it. He even raised awareness to this issue in a 2008 editorial in Archives of Internal Medicine (now JAMA Internal Medicine), written with Victoria Persky, titled "The Canary in the Coal Mine of Coronary Artery Disease." They were reacting to a study of 3,237 autopsy findings from 1981 through 2004 in Olmsted County, Minnesota. Within the study, coronary artery disease decreased in the 1980s; decreased more slowly in the 1990s; and increased after 2000. "The results are alarming enough to alert public health officials to begin monitoring younger cohorts for early signs of CAD with much greater vigilance."
This week Olshansky was more blunt. "The canary in the coal mine has died," he told me.
The Overlooked Aspect: Frailty
"If you look at the general health status of the population from national health surveys, what they found was exactly what we found years ago: the health status of the population is not good among baby boomers, basically 45 to 64," Olshansky says. "We've known that they've been more frail, and more disabled than previous generations passing through the same age. Precisely why that is the case, in part, is what these authors helped to identify."
Increased frailty comes up in Case and Deaton's study, though it's been less remarked upon than the death rates.
There was a large and statistically significant decline in the fraction reporting excellent or very good health (6.7%), and a corresponding increase in the fraction reporting fair or poor health (4.3%)…. On average, respondents in the later period reported an additional full day in the past 30 when physical health was "not good."
The increase in reports of poor health among those in midlife was matched by increased reports of pain…. One in three white non-Hispanics aged 45–54 reported chronic joint pain in the 2011–2013 period; one in five reported neck pain; and one in seven reported sciatica. Reports of all four types of pain increased significantly between 1997−1999 and 2011−2013…. The fraction of respondents in serious psychological distress also increased significantly.
[…] Over this period, there was significant midlife deterioration, on the order of 2–3 percentage points, in walking a quarter mile, climbing 10 steps, standing or sitting for 2 [hours], shopping, and socializing with friends. The fraction of respondents reporting difficulty in socializing, a risk factor for suicide, increased by 2.4 percentage points.
And on, and on, and on. Physical and mental frailty can have a mutually reinforcing relationship, and it makes sense that increased amounts of both would correlate with substance dependence—especially painkillers—and mortality. But where is the frailty itself coming from?
Case and Deaton suggest that increasing inequality, and the United States's unusually weak safety net among developed countries, plays a role. The correlation is certainly strong, and we now know a lot more about the mental and physical effects of stress on the body. Financial and other stresses are obviously prevalent among blacks and Hispanics, but, as Case and Deaton write, "many of the baby-boom generation are the first to find, in midlife, that they will not be better off than were their parents." Perhaps the relative level of disillusionment, for whites, plays a role?
Still, that's a lot of specific physical pain—specific increases in joint, neck, and back pain. Intuitively, it's the kind of pain one associates with intense physical labor, but that kind of labor has generally been in decline among the white working-class. I mentioned this puzzle to Olshansky.
"I've had some people today contact me by email, saying that we need to look more closely at the health status of veterans, especially coming back from conflicts overseas. These are all younger men and women in their 20s, 30s, 40s, and 50s, who are coming back with levels of frailty and disability, both physical and mental, in ways we've never seen before," he says. "There's a lot going on in the dynamics of these groups moving through the age structure and getting older, that have yet to play themselves out in ways that we fully understand."


