The talk of the wonks today is a new NBER working paper paper on infant mortality in the United States, co-authored by the influential young University of Chicago economist Emily Oster, herself the author of a recent book on pregnancy that I've been meaning to get to.
If people are talking about it, you might have guessed that the news is not good. And broadly speaking, it's not. In 2013, according to the CIA World Factbook, the United States ranked 55th in infant mortality, at 6.17 per 1,000, between Poland and Serbia. (The range is quite wide—117 in Afghanistan to 1.81 in Monaco, the only country under two per thousand.) It's closer to wealthy-but-developing countries like Qatar and the Cayman Islands than its fellow first-world major democracies, like France (3.31) and Japan (2.13).
There are different ways of calculating it, as Aaron Carroll writes, in which America's numbers are not as bad. But: "reporting differences (the favorite explanation of those defending the US healthcare system from the infant mortality metric attack) explained up to 40% of the disadvantage in US infant mortality. But that would only get us closer. It would still leave us way worse."
The picture is not wholly negative, and that's where the paper gets interesting. Oster and her co-authors, Alice Chen of USC and Heidi Williams of MIT, observe that neonatal mortality rates are similar to their comparison countries, Finland (which has a tremendous reputation for early-childhood care) and Austria. The rates are also comparable to Austria and Finland in terms of low-birthweight infants throughout the first year.
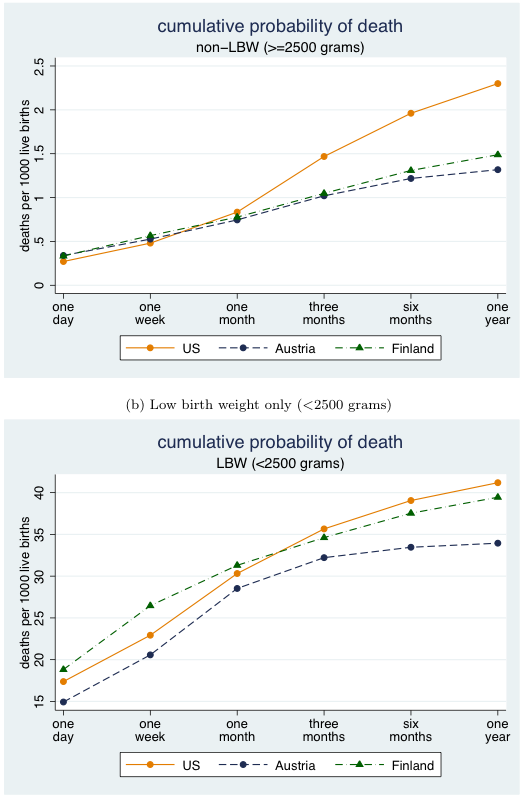
Altogether it looks like this (from 2000-2005):
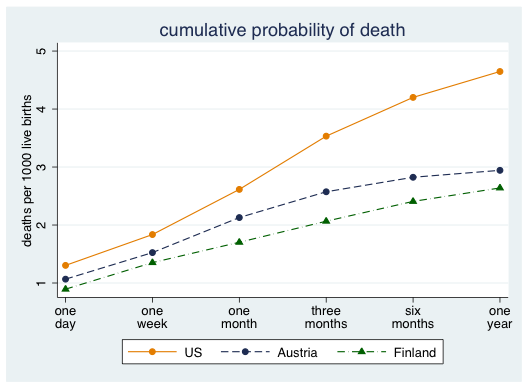
In other words, the U.S. health care system is comparatively good, compared to the selected peers, at addressing the needs of infants when they are at their most vulnerable—from one day to a week overall, and throughout the first year in terms of low birthweight infants.
But go back to that first non-LBW chart. Things are good, roughly speaking, up to one month. Then it goes haywire. It's odd—the system starts to fail as children get less vulnerable.
Or, in their words: "the US neonatal mortality disadvantage is quantitatively small and appears to be fully explained by differences in conditions at birth. In contrast, the US has a substantial disadvantage relative to either Finland or Austria in the postneonatal period even in our comparably reported sample and even conditional on circumstances at birth…. If we condition on birth weight as a measure of health at birth, the US actually has an advantage in the first month of life relative to either Austria or Finland, but retains a disadvantage in the postneonatal period."
Even further, the authors write that "less advantaged groups in the US do better than their counterparts in Europe conditional on circumstances at birth." So… that's good, unquestionably. Problematic as the American medical system is, it's sophisticated, and appears to be effective for the delicate work of neonatal/low-birthweight treatment.
The paradox is that it doesn't appear to work as well when that work should be easier—and it doesn't work for the poor:
We show that infants born to white, college-educated, married women in the US have mortality rates that are essentially indistinguishable from a similar advantaged demographic in Austria and Finland.
But:
Given that one of the most striking facts about infant mortality in the US is the disparity in mortality between black and white infants, it is important to note that the facts we document in this paper are essentially unchanged if we exclude US blacks from the sample.
What are they doing well that we're not doing? The authors suggest home nurse visiting programs as a tested method. The Finns actually send a care package to every mother in the country, and have been for over 75 years, initially to low-income mothers but now to all mothers (one theory in political/social science is that programs available to most or all of the population will inevitably work better because they'll get more support).
The "maternity box" contains lots of stuff—clothes, all-useful muslin cloths, bath thermometer, a snowsuit for the country's freezing weather, a picture book to encourage reading—but the box is arguably the most important part:
"Babies used to sleep in the same bed as their parents and it was recommended that they stop," says Panu Pulma, professor in Finnish and Nordic History at the University of Helsinki. "Including the box as a bed meant people started to let their babies sleep separately from them."
An infant sleeping in a cardboard box might seem kind of depressing, but it gives parents a sleeping setup specifically for an infant, meant to prevent both suffocation (an issue that's reared its head recently in the U.S.) and bedding kludged together from around the house that can also present a risk. Finland, as Olga Khazan details, is simply very good at its childhood safety net.
Richard Mayhew, a knowledgeable writer on the American health care system, writes that "we have a bias towards heroism and not towards maintaining good health," by way of explaining how we're quite good at taking care of extremely vulnerable newborns but not at problems requiring a lower degree of difficulty. Those require less intellectual and medical might, but the same dogged determination.