I was digging around for data on measles vaccinations in Illinois when I came across Project Tycho, a massive, Creative Commons-licensed store of health data with a wealth of historical information. Such as cases of measles in Illinois over the 20th century, which revealed a measles scare I'd never known, even though I was at a vulnerable age at the time.

In 1963, the measles vaccine was licensed in the United States. It worked extremely well, as the graph suggests, though it still had room for improvement in the 1970s (one theory is that a heat stabilizer introduced in 1979 prevented failure from improper storage). After that, its efficacy runs north of 95 percent and measles cases peter out to a bare minimum.
But then there's a big resurgence around 1989. "Big" in relative terms perhaps—tens of thousands of cases compared to hundreds of thousands prior to the vaccine—but still far more than the then-low of 1,500 cases nationwide in 1983. And Chicago was one of the hardest-hit cities.
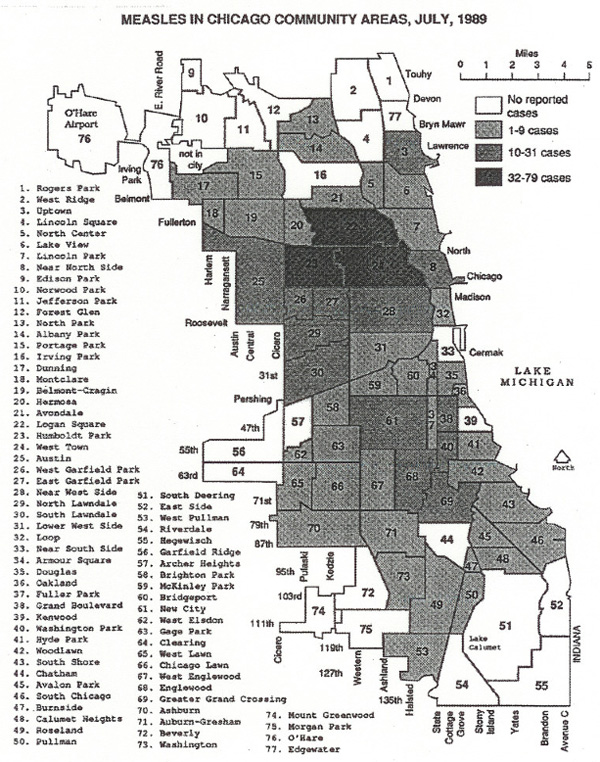
There were 2,232 cases in Chicago in 1989, ten times the then-national rate for that year. Compare that to thirty-seven nationwide in 2004, or even numbers that have people worried now—644 in 2014.
As you can tell from the map, measles hit Chicago's poorest neighborhoods the hardest, and in particular neighborhoods with large Hispanic populations. A Tribune piece from July of that year gives a sense as to why:
Laura, who moved with her family to Chicago about three months ago, was not vaccinated while she lived in Mexico. Now she lies hooked up to an IV in a mustard and yellow room at Norwegian-American Hospital in the Humboldt Park neighborhood.
"I thought she was going to die," Manriquez said, while holding her daughter's hand. "I was desperate."
[snip]
Dr. Michael Fisher, medical director of the Erie Family Health Center, said the center's four sites on the Near Northwest Side have treated more than 20 cases of measles.
"It's common in inner-city poor communities," he said. "People in the community we take are less likely to be vaccinated. They're poor. They don't have a green card [work authorization]. They may not get preventive care. There are language barriers."
Norwegian-American had to open a measles ward in June, after the prior month it treated 21 patients in a 260 bed hospital, with another 22 outpatients. As the number of cases climbed towards the thousands, the city's health department went door to door in the Robert Taylor Homes with vaccination kits, and set up booths at summer festivals. Vaccination rates in neighborhoods like Humboldt Park were extremely low:
Because nearly 75% of reported patients were unvaccinated, the CDH reviewed records to estimate the percentage of children entering kindergarten who had been immunized for measles by 2 years of age. The survey included 32 public and 14 parochial schools in 10 communities with high measles incidence rates and eight public or parochial schools in four areas with low incidence rates. In 32 public schools for which student racial characteristics were available, enrollment was classified as predominantly white, black, or Hispanic. An average of 80% of students in schools with predominantly white enrollment had received measles vaccine by 2 years of age, compared with an average of 50% and 52% of students in schools with predominantly Hispanic and black enrollment, respectively. An average of 27% and 29% of students in schools with predominantly black and Hispanic enrollment, respectively, first received measles vaccine the year of school entry (at 4-5 years of age), compared with 7% of students in schools with predominantly white enrollment.
The CDC attributed the nationwide outbreak, which wasn't brought fully under control until 1991, to unvaccinated preschoolers, and to school-age children who had received only one dose of the vaccine (one of the worst-hit places in the state was Bradley University in Peoria, where 110 vaccinated students caught the virus in early 1989). So, in 1989, the CDC's Advisory Committee on Immunization Practices officially recommended a second dose. The next year, the state of Illinois required all new fifth-grade and college students to show evidence that they'd received two doses. In 1991, the number of measles cases fell to 27 statewide, down from 3,213 in 1989. 10 people in Illinois died during 1989 from measles, about a quarter of the nationwide total.
As of 2013, the CDC reported that 88 percent of 13-17 year olds in Chicago living below the poverty line had at least two doses of the measles/mumps/rubella vaccine, just three percent lower than those above the poverty line. The racial difference is still significant—98 percent among white adolescents compared to 87 percent among blacks and 86.4 among Hispanics. It's still not as high as is recommended, since measles is so contagious, but it's a huge increase from the situation in 1989 that fueled the epidemic.
Measles has technically been eliminated in the United States since 2000. But it really wasn't that long ago that an epidemic tore through some of the nation's biggest cities—well within my lifetime. That I'd completely forgotten, or never even heard of it until it showed up as a blip of data, suggest how easy it is to forget, and to forget the lessons of herd immunity.



