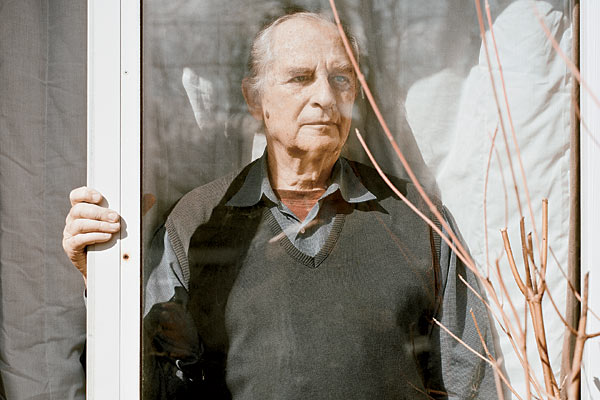
Jerry Dincin awaits his “exit” at his Highland Park home in early March.
In February, as temperatures in the Chicago area unseasonably spiked into the 60s and 70s, Jerry Dincin’s neighbors took to the streets. They strolled around the North Shore town of Highland Park wearing T-shirts and shorts, with their dogs and children, soaking up the sun. Everyone, including Dincin, a retired psychologist, marveled at how nature can surprise us. But for him, the beauty was bittersweet. “I think this is my last winter,” he told me, staring through a window at the bright blue skies.
At 81, Dincin does not want to die. He loves Susanne, his wife of 11 years; her son, Ben, who starts college this fall; and his four adult children from a previous marriage. And his cats Sparky (the fat one) and Scrappy (the skittish one). And the symphonies of Beethoven. And the wooden objects he and Susanne collect at art fairs and hang on the walls of their red-roofed ranch house. He is in no hurry to leave all this behind.
But there is the cancer, diagnosed just two weeks after his honeymoon with Susanne at Niagara Falls. Dincin has undergone radiation and blood therapy in a futile effort to stop the spread from his prostate to his ribs, to his spine, to the bony girdle of his pelvis. He has tried prescription drugs, marijuana, acupuncture, and hypnosis for the pain and enfeeblement that followed. The cancer will immobilize him, the doctors say, and then it will kill him. There is no debating this.
Since early this year, Dincin has been spending his remaining time with family, reading courtroom dramas, getting medical treatment, and trying to manage his increasing pain. But in May some news from the state of Minnesota interrupted that routine. The Dakota County Attorney’s Office had indicted him for assisting in the 2007 suicide of Doreen Dunn, a 57-year-old mother from suburban Minneapolis.
For as it turns out, Dincin is far from the typical North Shore retiree. He is one of the nation’s most prominent right-to-die advocates. From 2009 to 2011, he was president of the Final Exit Network, a controversial nonprofit group that aims to help the terminally ill and those suffering from unbearable pain who want to choose when their lives end. He says that he has been present with 14 such people, including Dunn, during their self-inflicted deaths. Dincin calls the right to die “the ultimate civil right.”
“To me, living an extra week or an extra month in bad condition just isn’t worth it,” he says. “I know that a lot of people don’t feel that way. A lot of people feel that, you know, the last drop of life, you should squeeze everything out of it. But I don’t think so.”
Now that he faces his own death, however, acting on that belief has become agonizingly difficult. “I’ve been very concerned about my own courage and being able to take my own life with my own hand,” he says. “I spend a lot of time thinking about it. Too much time.” He pauses. “I’m intellectually convinced that’s exactly what I want to do. But actually [doing it] is . . . it’s a big deal when you don’t want to die.”
* * *
Dincin opens the door before I can knock and shakes my hand. We’ve spoken by phone half a dozen times over the previous few years, but he is not quite what I imagined. Strong looking, for one thing—six feet tall, 195 pounds—with thinning gray hair pulled back into a bohemian ponytail. His blue eyes are faded but full of life. He looks pretty good, considering the war going on inside his body. It’s mid-February.
Today the pain in his back is a three, he tells me. (Dincin assesses his pain level on a scale from zero to ten, with zero undetectable and ten unbearable.) Just days before, he had finished his latest treatment: A cup of his blood was removed, flown to California, treated with an immunotherapy drug called Provenge, flown back, and returned to his body through a vein in his arm. It won’t cure him, but he hopes it will buy some quality time.
Sitting in his sunny living room, we talk about his life and death over a bowl of fresh berries. Despite having spent most of the last five decades in Illinois, Dincin speaks with a native Brooklynite’s accent. “I thought it [the decision to die] is a lot easier than it is,” he says, choosing his words carefully. “I love my wife. I want to stay with her, and she wants me to live.”
Still, Dincin doesn’t want to end up on an IV in a hospital or a nursing home, pumped full of potent drugs, strange to the strangers taking care of him, strange to his family and friends, strange even to himself, whatever part remains. Nor does he want to suffer great pain. So he resolves that he—not cancers, or gods, or doctors—will choose the day, the time, and the way he exits the world he loves. He will die when the pain becomes too much.
I ask Susanne how she feels about her husband’s decision. She sits alone on a couch, sipping tea—a bespectacled psychotherapist used to having hard conversations. “It’s his life,” she says quietly. “Jerry’s a strong man. He has a very strong personality, and he doesn’t do well being weak. If he were to get into a very incapacitated state, he would be a very grumpy guy. I understand this.”
“More than grumpy,” Dincin corrects.
“I saw with my parents,” Susanne continues, “there comes a point where the quality of life is not great.”
“I’d like to die in my sleep,” says Dincin, “but that’s not going to happen.”
A lifelong atheist, Dincin doesn’t feel bound by any religious prohibition against suicide. “I understand why people buy into an afterlife,” he says, “to know that you’re not really dead, that you’re going somewhere else where you’ll meet your parents and grandparents. It’s a terrific invention. I just think it’s bullshit.”
* * *
Photograph: Daniel Shea
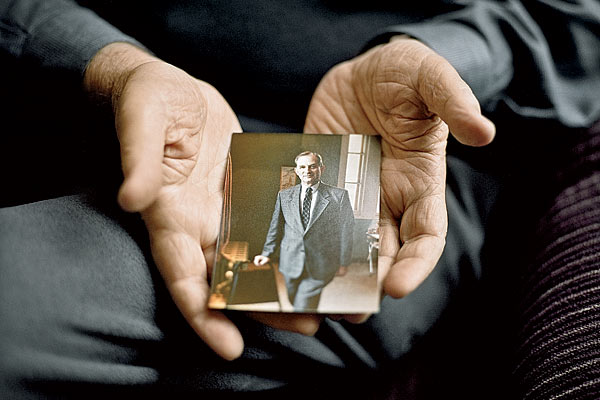
Dincin holds a photo of his younger, healthier self
Dincin’s first experience with death was his father’s sudden heart attack when Dincin was 16. By the time he rushed home from summer camp, the old man was gone. He and his mother wound up taking over his father’s furniture business in Manhattan.
Eventually Dincin earned a bachelor’s degree from Brooklyn College and a master’s in social work. He took a job in psychiatric rehabilitation—helping people with mental disorders adjust to daily life—in New York City, then started two similar programs in New Jersey. In 1965, he moved to Chicago to head Thresholds, a social service agency in Ravenswood that assists the mentally ill. While running Thresholds, Dincin got his Ph.D. in clinical psychology from Northwestern University.
He couldn’t have done it without Susanne Streicker, a blond 20 years his junior who grew up in Evanston: Working as his assistant, she helped him research his dissertation. Streicker ultimately became a supervisor at Thresholds before leaving in 1989 and adopting children. Although he talked to her once in a while, Dincin didn’t see her again until 1999. Not long after separating from his first wife, he ran into Streicker at a mental health conference in Minnesota. “We just struck up a good friendship,” he says. “And it’s worked out beautifully.”
After his cancer diagnosis at age 70, Dincin retired from his job. A few years later, he found himself drawn to the right-to-die movement.
He stumbled across an article about the Hemlock Society of Illinois in the Chicago Tribune and learned its history. Derek Humphry, author of Final Exit: The Practicalities of Self-Deliverance and Assisted Suicide, had founded the society in 1980 to counteract assisted suicide restrictions in America, through both legislation and individual counseling. The Final Exit Network emerged from Hemlock, becoming a nonprofit in 2004. Today it claims 3,000 members nationwide, about 200 of them in Illinois.
Dincin had always been interested in issues of social justice. His illness “triggered a sense of apprehension about dying, something I’d never felt,” he recalls. “I wanted the right to die when I chose, and I felt others should have that right too.”

Dincin with his wife, Susanne, in 2005, after swimming with seals in the Galapagos Islands.
While some other right-to-die groups, such as Compassion and Choices, focus on legislative advocacy, FEN takes a personal approach. It shows people in the agonies of terminal illness or chronic pain how to die on their own terms. The group claims to have helped some 200 Americans die over the last decade: sufferers from cancer, multiple sclerosis, emphysema, Parkinson’s, and other diseases they could no longer endure.
FEN members stress that they are not executioners in the mold of the late Jack Kevorkian, the polarizing medical pathologist and assisted suicide activist who used a DIY machine to help 130 people end their lives. Instead, they cast themselves as end-of-life advisers, protected by the First Amendment, who offer guidance and emotional support to those with “intolerable suffering.” Deaths are referred to as “exits”; the counselors are “exit guides.”
The group’s leaders say that they follow a lengthy interview process with prospective exit candidates, which can take months. A FEN-affiliated doctor examines each person’s medical history. If the candidate has exhausted every other option and proves to be mentally competent, one or more exit guides offer counseling on the easiest way to die and other end-of-life matters, such as whether or not to involve family. If the person requests it, the guides may witness his or her last moments on earth. “It’s the quintessence of compassion,” says Rosalie Guttman, a gerontologist in Hyde Park who currently leads the Illinois chapter of the Hemlock Society.
Dincin joined FEN in 2004 and became an exit guide in 2005. When I ask him about handling that role, what Dincin describes is somewhat clinical, along the lines of how a medical doctor treats patients: with compassion yet slightly detached. He mentions a woman with Lou Gehrig’s disease in Arizona and a woman with Huntington’s disease in Tennessee. But he says he can’t remember all of the exiting FEN members’ names, nor where most of them lived or what ailed them. Forgetting has helped him move on.
All told, Dincin says, he has witnessed 14 deaths. One of them, in May 2007, was Doreen Dunn’s.
Dunn had long been plagued with chronic pain due to complications from surgery some years before and had become a member of FEN in January 2007, according to prosecutors.
Medications reportedly did little to relieve her suffering. She was spending most of her time lying on the sofa of her home in Apple Valley, Minnesota. That’s where she was, watching TV, when Dincin and FEN’s former medical director Larry Egbert, a physician from Baltimore, arrived.
Dincin and Egbert sat with Dunn and watched her asphyxiate inside a plastic hood that she had connected to a helium tank, the way that FEN recommends exiting. It was over quickly. “I don’t think we were there for an hour,” Dincin says. “She wanted desperately to die, and I was just really there as a witness.”
Assisting a suicide is illegal in most states, though the criminal statutes vary. In Illinois, for example, giving physical assistance in a suicide is a crime, but giving advice is not; in Minnesota both are illegal. (Oregon and Washington allow terminally ill patients to end their lives by taking lethal medications prescribed by a physician; in 2009, the Montana Supreme Court ruled that “we find nothing in the plain language of Montana statutes indicating that physician aid in dying is against public policy.”)
Despite the fact that a 2005 Pew Research Center poll found that nearly half of Americans approve of it, physician-assisted suicide is firmly opposed by the American Medical Association and the American College of Physicians. It “is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks,” states the AMA’s official policy. Most major religions also forbid assisted suicide, by a physician or anyone else.
But FEN officials argue that what they do is not assistance. “We’ve worked for years to ensure that exit guides do not break the law,” says Robert Rivas, the general counsel for FEN. “They do not provide the means [or] any physical assistance. They provide only information and a supportive presence.”
That distinction was lost on Georgia authorities. In February 2009, they arrested FEN’s president at the time, Ted Goodwin, and three others, charging them with assisting in the suicide of a man suffering from oral cancer. Its attorneys argued that preventing people from learning about committing suicide violates freedom of speech, which is protected in the Constitution.
The argument worked. In Georgia and in Arizona, which had brought similar charges that same year, no FEN members who went to trial—including Goodwin—were found guilty.
As a condition of bail, Goodwin had to dial back his involvement with FEN. In February 2009, Dincin, who had been voted FEN’s vice president in 2007, replaced him as president. “I definitely did not want the president’s responsibilities,” he says, “[but] I felt that the best option for FEN to stay functioning was for me to assume those duties.”
* * *
Photography: (top) Daniel Shea; (right) courtesy of Dincin

In his Highland Park living room in March.
Two years and four months later, Dincin discovered that the prostate cancer that he had battled for nearly a decade had metastasized to his spine.
At first, ibuprofen was enough to manage his back pain. And for a while, he remained upbeat. He stepped down from the role of FEN president but still exercised lightly, took an adult education course about the brain at National Louis University, and gossiped with Guttman. (Dincin had become close friends with the gerontologist when they cohosted a Chicago public-access television show about end-of-life issues.)
Before our meeting in February, Dincin asked Guttman to be his exit guide. He could exit alone, of course, but he feels better knowing someone will be there. He plans to die the same way Dunn did. But he’ll be in his bedroom—not the living room, where Ben might find him.
He shows me a clear plastic hood the size of a grocery bag. It has a circular elastic strip at its open base. Just above the elastic is a hole that can fit a tube, which can then be connected to a helium tank.
Dincin pulls the hood halfway over his head. His blue eyes peer at me through the plastic. After a few moments, he removes it. “That’s it,” he finally says. “You just put it on the back of your head, plug the two ends of the tube in, make sure the tank is full, then pull it down over your face.”
He has pictured it countless times: sitting in bed, attached to the tank. Imagining turning the valve is hardest. It happens slowly, quietly. No Beethoven’s Ninth, or birds chirping outside, or Susanne’s voice to comfort him. “I can’t quite imagine what it’s like to be dead, even though I’ve been with dead bodies,” he says. “I can’t picture myself in that state.”
Susanne doesn’t want to be there when it happens, and Dincin doesn’t want that either. It’ll be bad enough for her to find him later in their bed, where she’ll still have to sleep. He also doesn’t want her questioned about his death or, worse, charged with it. He’s already penned the letter explaining what he’s done and why. He’s told his attorney, his accountant, and the couple’s stockbroker. He has prepaid for his cremation and put labels on the Mason jars that will hold his remains. He knows what can happen when preparations aren’t made.
In late February, Dincin tells me that his pain level is at five and rising. A month later, Susanne e-mails me that he is doing poorly; the sensation in his back is, at times, a ten: “He has started on radiation, which helped alleviate the pain, but he is very weak. He still has a few more radiation sessions. He has been on steroids to help with the pain, but Jerry did not tolerate that well.”
Dincin briefly stops responding to my e-mails. His children make what they think might be their final visits. He spends as much time with Susanne as he can. He tells Guttman to be ready.
On April 3, Dincin and Guttman have a long chat on the phone. He is weak, he tells her, and can hardly move across the room—ten steps feel like ten miles. Given this decline, he finally sets a provisional date to make his exit: May 4. She tells him that it doesn’t have to be set in stone.
Dincin’s last radiation treatment ends on April 7. A week later, he e-mails: “[It] left me washed out and completely without energy. I am slowly recovering from that, but woke up on Saturday with another cancer poking at me from my rear shoulder. The drama thickens, and I don’t like it.”
On May 2: “Very strong side effects from radiation—dizzy-cant walk-stay at home—weary weary at the slightest movement.” However, he adds, “right now no pain from the cancer itself.”
So Dincin postpones his May 4 exit, clinging to the time he has left.
* * *
Little more than a week later, on May 11, comes the news from Minnesota: Dincin and three other people affiliated with FEN—Goodwin, Egbert, and case coordinator Roberta Massey—are under indictment, as is the organization. Dincin is charged with one count of “advising, encouraging or assisting” in a suicide and one count of conspiracy to do so, both felonies. He is also charged with interfering with a death scene and conspiracy to do so, which are misdemeanors. Under Minnesota sentencing guidelines, “the maximum penalty for someone with no criminal history convicted of aiding suicide would be up to a year in jail and a fine determined by the court,” says James Backstrom, a prosecutor with the Dakota County attorney’s office. FEN also faces possible fines.
The delay in filing indictments—it has been five years since Dunn died—stems in part from the difficulty of pinpointing helium asphyxiation as a cause of death. Helium kills by displacing oxygen in the body, leaving no trace. An autopsy concluded that Dunn had died from natural causes. Two years later, Georgia officials told law enforcement in Minnesota about their investigation into an assisted suicide case. That led Backstrom to connect Dunn and FEN.
The charge that he assisted Dunn’s suicide is “just a final irony,” Dincin says. “I gave her no affirmative advice. I gave her no encouragement.” As for the charge that he removed the helium canister and tubing from Dunn’s house: “Since we didn’t think we were committing a crime,” he says, “we saw no reason why we couldn’t remove it.”
At presstime, the defendants’ initial appearance was scheduled for July. While Backstrom says he could seek to extradite Dincin to Minnesota, “It could be possible for Dincin to testify, if he chooses to do so, by video deposition.”
But Dincin isn’t wasting the time he has left worrying about legal proceedings. “I have no intention of going to Minnesota to defend myself in person, and I have medical backup for that,” he says. “If my situation gets bad enough, I will take the final exit that I have planned. And if it doesn’t, I will sit and listen to the trial as much as I can.”
No matter the outcome of the case, Dincin doesn’t feel guilty about his participation in Doreen Dunn’s death or in any of the others. “I mean, I can’t say that I was happy that she died,” he says. “But I would say that I was glad that she was out of her misery. Because she wanted to be out of her misery.”
He will know when it is his time, just as he says Dunn knew when it was hers. Until then, Jerry Dincin is just happy to be alive.
Photograph: Daniel Shea


