
House M.D was one of my favorite shows for a long time, at least until it stopped being a pleasantly repetitive, formulaic vehicle for Hugh Laurie's showboat acting and introduced a bunch of new actors in order to become "character driven." The best-known of those characters, mostly because she's played by the comely Olivia Wilde, is Remy Hadley, a doctor whose mother died of Huntington's, and a central plot point for part of the show is her avoidance of getting tested for the disease. Since it's a neurodegenetive disorder, the genetic dominance of which gives the children of sufferers a 50 percent chance of developing it, she refuses to get tested for fear of what the knowledge would do to her, at least until Dr. House (naturally) diagnoses and pushes her to get tested.
This is about when the show starts to go into decline. But: it turns out there's some logic to her avoidance, according to a study by Emily Oster, a gifted young economist at the University of Chicago. Oster and two co-authors used a set of Huntington's sufferers to examine what people do when they know they're probably going to die early—symptoms usually begin during the mid-30s to mid-40s, and suggest a typical lifespan of another 20 years. In other words, sufferers of Huntington's can be expected to die a decade or two early, as the average U.S. lifespan is 78.5 years; according to Oster's paper, the life expectancy for Huntington's patients is around 60 years.
So Oster asked: how do people respond? Having a future, but a shortened one, means you don't plan for it (PDF):
Earlier symptom onset is associated with less education. Relative to individuals with no symptoms by 30, those with symptoms between 15 and 18 are less likely to begin college and much less likely to complete it. Individuals with symptoms between 19 and 22, and between 23 and 28, are no less likely to start college but less likely to complete. The eff ects scale with age of onset, indicating divergence of educational investment as HD status is revealed. The analysis of job training demonstrates similar results, even controlling for occupation.
Keep in mind that someone with Huntington's at 19 will probably live until around 40. So the effects of college or job training would still pay off, though over a shorter period. So it does raise an interesting question: what's the effect of having less payoff over the years on getting a college education or job training? The effect Oster found was substantial:
A simple comparison of means suggests a large impact of test results on educational attainment. Individuals who learn through genetic testing that they carry the HD mutation get, on average, 14.3 total years of schooling and 36% of them complete a bachelor degree. In contrast, those who learn they have a negative test result get an average of 15.03 years of schooling and 63% of them complete a bachelor degree.
[snip]
Our outcome of interest is job training for advancement or promotion, and we fi nd very large impacts. Relative to those with no symptoms by 40, individuals with symptom onset between 20 and 30 are about 27 percentage points less likely to report any job training for advancement or promotion. Individuals with symptom onset between 31 and 40 are also less likely to undertake training for advancement, although the coeffi cient is smaller, which is consistent with the fact that these individuals could have undergone job training in their twenties.
The implications for this are pretty interesting. Way more people in the U.S. go to college now than they used to. Oster suggests this is related to increasing life span:
We document the importance of life expectancy in explaining the 1960 versus 2010 di fference, as well as the 1980 and 2000 versus 2010 diff erences. Changes in life expectancy account for a moderate share of the diff erences—between 6 and 20%, depending on the time frame. In the most recent decade it seems that increases in life expectancy play a relatively smaller role in the continued growth in college-going.
I.e. since the returns from college are greater (because we're living longer), people are more likely to go to college.
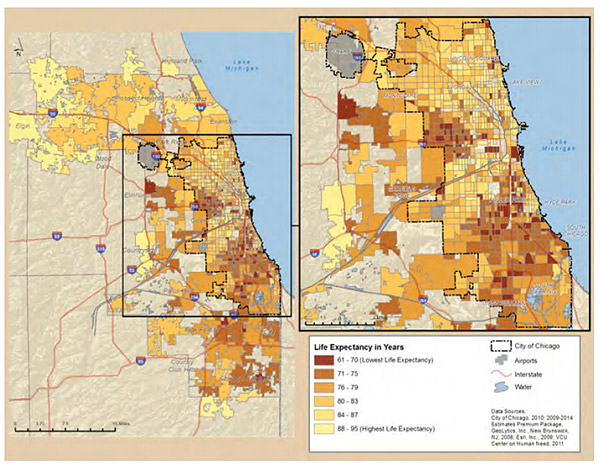
What this put me in mind of was some research on life expectancy in Chicago: "people living in Chicago neighborhoods with a median income higher than $53,000 a year have a life expectancy almost 14 years longer than Chicagoans who live in communities with a median income below $25,000." There are a handful of Chicago neighborhoods where life expectancy is 61-70 years old, a bit higher but in the ballpark of Huntington's victims (PDF).
It also reminds me of the idea of poverty as a health issue that Steve Bogira of the Reader has been writing about:
A measure called Years of Potential Life Lost factors in the prematurity of deaths like homicide—and shows more compellingly the disparate impact of homicide on Chicago's poor black neighborhoods. In Chicago as in most places, a base age of 75 is used in calculating YPLL. A death at age 70 is five years of potential life lost; a death at age 25 is 50 YPLL.
In the five poorest neighborhoods, the YPLL rate for homicide was 2,172. That is, for every 100,000 residents, 2,172 years of potential life were lost each year to homicide. In the five least-poor neighborhoods, the YPLL rate for homicide was just 186.
It's not a one-to-one comparison, but I think Oster's research speaks to the tight relationship between poverty, health, and education—people are more likely to pursue education if they think they'll live long enough to really benefit from it.


