S. Jay Olshansky, an epidemiologist at UIC, published a study last month looking at lifespans in terms of race and educational level in the U.S. At first glance, the conclusions are not surprising:
Despite advances in health care and increases in life expectancy overall, Americans with less than a high school education have life expectancies similar to adults in the 1950s and 1960s.
"The most highly educated white men live about 14 years longer than the least educated black men," says S. Jay Olshansky, professor of epidemiology at the University of Illinois at Chicago School of Public Health and lead author of the study. "The least educated black women live about 10 years less than the most educated white women."
The differences are still significant; Steve Bogira has written about comparative lifespans in Chicago, for instance. But this may come as a surprise:
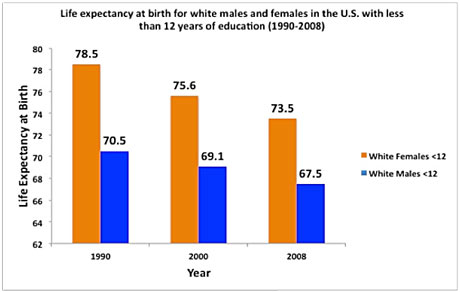
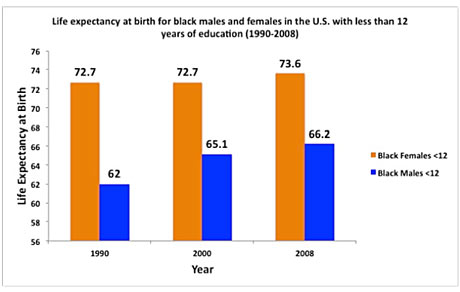
Black men and women without a high-school education have made modest gains in life expectancy over the past couple decades. The life expectancy among similarly educated white men and women, however, has declined—to the point where black women now outlive white women in their educational cohort. Hispanic life expectancies in the same group have also increased. What's behind the decline? When I saw the headline on Friday, despite being sick and completely out of it, this was the first thing that came to mind, having grown up in southern Appalachia in the foothills of the opiod belt:
James Jackson, director of the Institute of Social Research at the University of Michigan and an author of the new study, said white women with low levels of education may exhibit more risky behavior than that of previous generations.
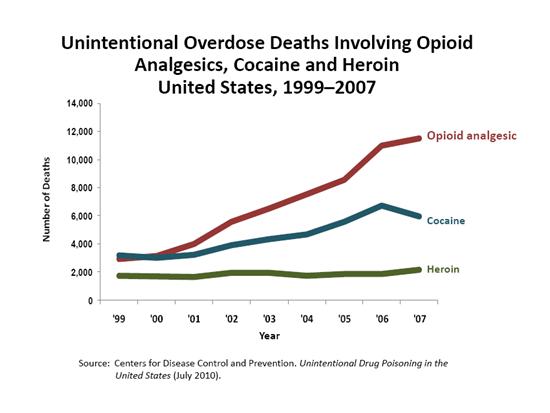
Overdoses from prescription drugs have spiked since 1990, disproportionately affecting whites, particularly women. Professor Miech, of the University of Colorado, noted the rise in a 2011 paper in the American Sociological Review, arguing that it was among the biggest changes for whites in recent decades and that it appeared to have offset gains for less educated people in the rate of heart attacks.
Opiod analgesics have outpaced other drugs in terms of overdose deaths:
Meanwhile, drug overdose deaths have spiked:
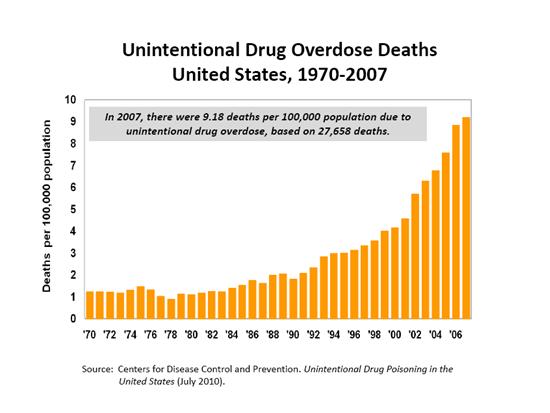
Meanwhile, suicide has passed traffic crashes as the leading cause of injury mortality in the United States (PDF):
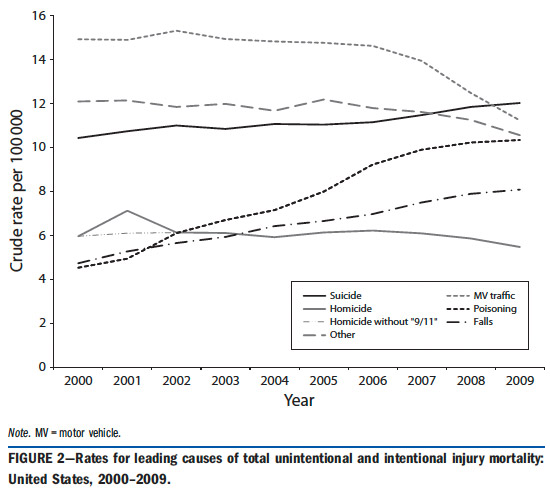
"Poisoning" includes opiate overdoses:
Unintentional poisoning exhibited by far the largest rate increase among the 5 leading causes of injury mortality. In 2008, drug overdoses represented 75% of unintentional poisoning deaths nationally, with prescription drugs representing 74% of the share. Moreover, overdoses of prescription opioid analgesics represented 74% of the prescription drug-related deaths, with this share increasing.
Which break along racial lines:
Two of the national studies examined racial/ethnic differences in unintentional injury mortality trends. The first study found an increase in the rate between 1992 and 2002 for non-Hispanic Whites and a decline for minorities. The second study reported a change in the unintentional injury mortality rate between 1999 and 2005, an increase, for non-Hispanic Whites only. Both studies reported excess rate increases for this group in various unintentional causes, most notably poisoning and falls.
While the link isn't definitive, the numbers suggest opioid overdoses as a cause. But there are likely others. Olshansky actually warned about these trends in 2005, in his paper "A Potential Decline in Life Expectancy in the United States in the 21st Century." Then, he pointed towards obesity and diabetes as concerning trends (emphasis mine):
A central problem with the [Social Security Administration's] forecast is best illustrated by its projections for diabetes. From 1979 to 1999, rates of death from diabetes increased annually by an average of 2.8 percent for males and 1.8 percent for females. In 1990, diabetes decreased life expectancy by 0.22 year for males and 0.31 year for females, but the negative effect of diabetes on life expectancy has grown rapidly since then. However, the negative effect of diabetes on the life expectancy of the population could now be several times as great as it was in 1990. Given the rapidly rising prevalence of diabetes and the prospect that childhood obesity today will probably accelerate the rising prevalence of diabetes in the coming decades, it is difficult to justify the SSA's assumption that rates of death from diabetes will decline by 1.0 percent to 3.2 percent annually throughout the 21st century, beginning in the year 2010.
[snip]
Unless effective population-level interventions to reduce obesity are developed, the steady rise in life expectancy observed in the modern era may soon come to an end and the youth of today may, on average, live less healthy and possibly even shorter lives than their parents. The health and life expectancy of minority populations may be hit hardest by obesity, because within these subgroups, access to health care is limited and childhood and adult obesity has increased the fastest.
At least through 2008, however, life expectancy among whites at the lowest educational levels has declined. There are similar problems of obesity, poverty, and access to health care—West Virginia suffers from both high obesity and prescription-drug abuse—but the numbers suggest that opioid abuse plays a role.
Plus: Olshansky on the "two Americas":



